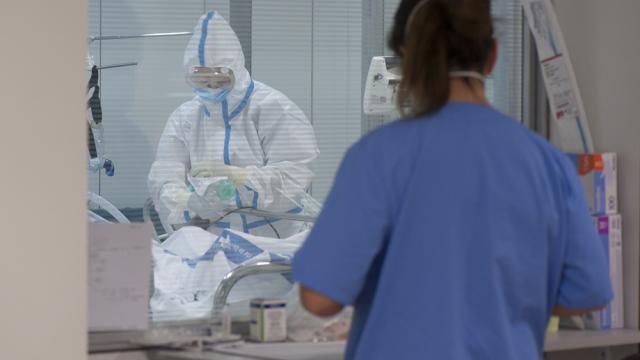
During the pandemic, several organizational changes were promoted at Bellvitge University Hospital: the critical care units of Intensive Care Medicine and the critical care units of Anesthesiology-Emergency Resuscitation (REA) and Surgical Resuscitation (RPQ) were moved to the area of Major Outpatient Surgery operating rooms, and the critical beds available for surgical patients were significantly reduced. Other measures included preoperative screening for SARS-CoV-2 and enabling clearly differentiated areas of the operating room area: Covid operating room (a specific Covid operating room was used for emergency surgery patients with positive RT-PCR), Covid-free operating room, and Covid-free critical area.
Different entry and exit routes were used for the operating room area and Covid-free critical area, in order to ensure that the operating room area was safe for surgery and postoperative and critic management. A protocol for airway management and the use of personal protective equipment were also implemented, which is mandatory for all staff involved in operating rooms and critical care units located in the surgery area.
Researchers from the IDIBELL and HUB perioperative pathophysiology and pain research group have conducted a study on clinical care in the surgical area during the first peak of the SARS-CoV-2 pandemic. The results show that in the pre-pandemic period, from January 13 to February 29, 2020, 1.649 hospitalized patients received surgery. During the Covid-19 period, from March 11 to May 15, 2020, 763 hospitalized patients were operated in the surgical area.
The percentage of patients with grade III to V complications according to the Clavien-Dindo classification was the variable used in the study to determine the non-inferiority of the Covid period to the prepandemic period. From samples of the two periods, a selection of patients was made based on the preoperative risk according to the ICD-10, considering the 3-4 degrees of preoperative severity, and depending on the background of the patients and the complexity of the surgery.
There were no differences in mortality or complications of Clavien-Dindo-grade III-V. Admission to the Anesthesiology Critics Unit was 64% in the Pre-Covid-19 period and 44% in the Covid-19 period, a significant reduction. Readmissions to the Critics’ Unit during the postoperative period did not show significant differences: they were 5.1% in the Pre-Covid period and 4.4% in the Covid period.
The reduction in critical critical care beds during the pandemic period clearly limited the number of major elective surgical procedures performed, while maintaining the same number of emergency procedures. However, late admission to the Anesthesiology ICU was similar in both periods.
According to the researchers, even if the number of critical beds is reduced, streamlining the use of available beds in the various ICUs should minimize the need to suspend elective surgery and should not be a limitation to scheduling more surgical patients.
The Bellvitge Biomedical Research Institute (IDIBELL) is a biomedical research center created in 2004. It is participated by the Bellvitge University Hospital and the Viladecans Hospital of the Catalan Institute of Health, the Catalan Institute of Oncology, the University of Barcelona and the City Council of L’Hospitalet de Llobregat.
IDIBELL is a member of the Campus of International Excellence of the University of Barcelona HUBc and is part of the CERCA institution of the Generalitat de Catalunya. In 2009 it became one of the first five Spanish research centers accredited as a health research institute by the Carlos III Health Institute. In addition, it is part of the “HR Excellence in Research” program of the European Union and is a member of EATRIS and REGIC. Since 2018, IDIBELL has been an Accredited Center of the AECC Scientific Foundation (FCAECC)