Researchers from the Bellvitge Biomedical Research Institute (IDIBELL) have found a new safe and effective method to reduce the duration of intravenous antibiotic therapy and the length of hospital stay for patients with community-acquired pneumonia. This strategy would help to optimize the care of hospitalized patients with pneumonia and reduce the hospital costs.
In Europe, pneumonia generates annual expenditure of 8.000 million euros; of this amount, more than half is heading for hospital care. The patients with community-acquired pneumonia requiring hospitalization longer than the average of patients admitted. The duration of stay in hospital is the most important component of the cost of the disease and also increases the risk of complications such as phlebitis, pulmonary embolism, and nosocomial infection. Researchers have reported considerable variation in length of hospital stay for patients with pneumonia, suggesting that physicians do not use a uniform approach to decide hospital discharge.
Often pneumonia patients remain hospitalized despite becoming clinically stable because they must complete the intravenous antibiotic treatment. The researchers note that the change from intravenous to oral therapy, when patients are clinically stable, can help to reduce their stay and the associated costs.
The researchers have designed a trial to test a new method more effective and economical than usual care. The new process will reduce the duration of intravenous antibiotic therapy and the length of hospitalization for patients. The method evaluated includes early mobilization and use of objective criteria for switching to oral antibiotic therapy and for deciding on hospital discharge or usual care. In this study, published in Archives of Internal Medicine, the researchers assigned 401 adults who required hospitalization for pneumonia.
New three-step method
The studied procedure is divided into three steps. The first is the early mobilization of the patient, from horizontal to upright position. This change improves the aeration and blood flow redistribution with optimized drug delivery for treatment of the infection. This reduces the risk of aspiration and it helps to maintain the functional health status.
The second step comprises the use of objective and simple bedside criteria for the early switch from intravenous to oral antibiotics. Finally, the third step is to use of objective criteria for clinical stability and to decide appropriateness for hospital discharge. Previous research has demonstrated that once stability is achieved in patients with pneumonia, the risk of severe clinical deterioration is 1% or less.
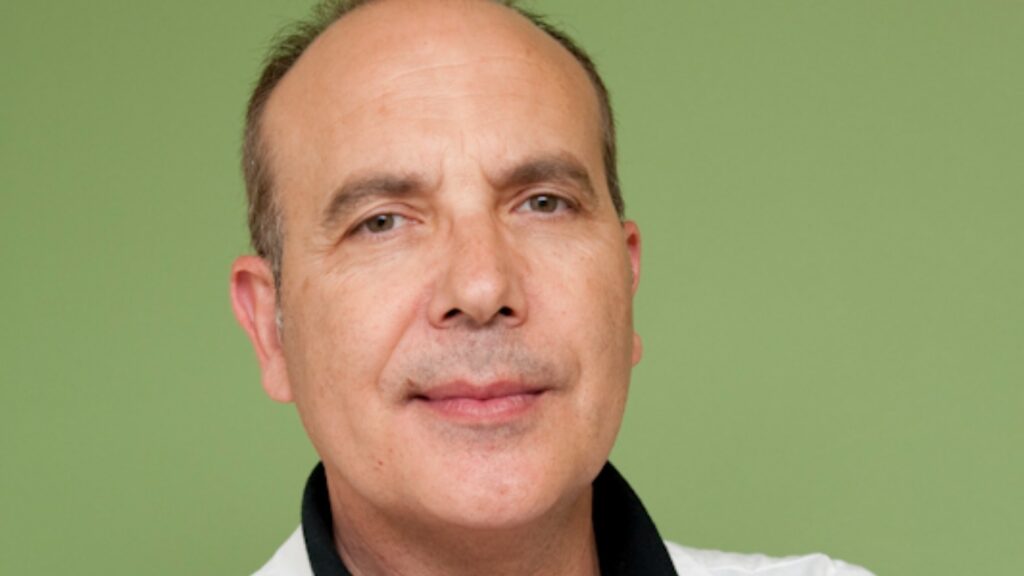
The researchers conclude that the use of this new three-step pathway is safe and effective in reducing the duration of intravenous antibiotic therapy and hospital stay for patients with pneumonia. The main researcher of this study, Jordi Carratalà, researcher and coordinator of the Infectious Disease in IDIBELL, Bellvitge University Hospital, notes that “this strategy will help optimize the process of care of hospitalized patients with community-acquired pneumonia, reducing hospital costs.”
Paper: Effect of a 3-Step Critical Pathway to Reduce Duration of Intravenous Antibiotic Therapy and Length of Stay in Community-Acquired Pneumonia. Carratalà J, Garcia-Vidal C, Ortega L, Fernández-Sabé N, Clemente M, Albero G, López M, Castellsagué X, Dorca J, Verdaguer R, Martínez-Montauti J, Manresa F, Gudiol F, Arch Intern Med. Published online May 21, 2012.