Researchers from the Genes and Cancer research group at the Bellvitge Biomedical Research Institute (IDIBELL) have identified inactivating mutations in a number of genes that code for HLA-I histocompatibility complex proteins, which are involved in the immune response and can condition the tesponse of lung cancer patients to immunotherapy. The study is a result of the collaboration between several national and international research centers, and has been published in the journal Clinical Cancer Research.
“Initially, we performed a genetic screening of lung cancer tumors using xenograft models, that is, human tumors that grow in mice, to obtain tumors with a low load of normal human cells,” explains Dr. Montse Sanchez-Cespedes, the last author of the paper. Sequencing of the tumors made it possible to identify several mutated genes, including some oncogenes and known tumor suppressor genes, and others that not previously described. “Among the latter, we were particularly interested in the B2M gene for its involvement in the functioning of the immune system, a target of new therapies developed for this type of cancer.”
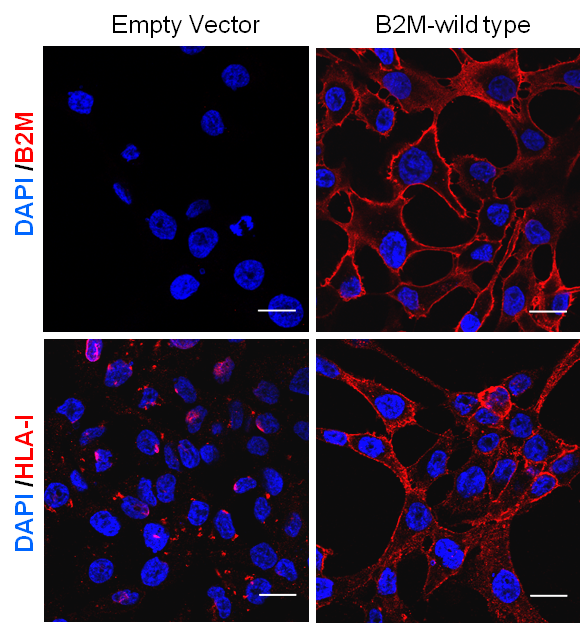
This observation was validated at a later stage using a large panel of lung tumors, determining that the frequency of B2M mutations in lung cancer is 6-8%. At the same time, the researchers demonstrated that de novo reintroduction of this gene into cell lines that were deficient in B2M restored the functioning of the HLA-I complex.
The new immunotherapy treatments aim to block the activity of certain proteins that inhibit the immune system. In lung cancer, this therapeutic option has yielded hopeful results in about twenty percent of patients. However, the treatment can only be effective if the tumor cell has a functional HLA-I complex.
Thanks to a collaboration with the Vall d’Hebron Institute of Oncology (VHIO), the IDIBELL team was able to work with samples from 14 patients undergoing immunotherapy to determine levels of B2M and other proteins or molecules related to the functioning of the HLA-I complex. “Despite having a limited number of samples, we were able to observe a clear trend: in those patients with tumors expressing high levels of these proteins the response to therapy was superior,” explains the researcher.
“In the near future, if we have enough samples, we would like to confirm the correlation between B2M expression and the response to treatment observed in this study,” notes Dr. Sanchez-Cespedes. “Likewise, we will try to find new genetic profiles or molecular components that can be used to determine the response of patients to immunotherapy other than the levels of B2M and PD-L1 (one of the targets of these treatments), and to characterize other genes related to these immune processes”.